Tajima Serial Connection Between Two
.jpg)
Adobe Flash Player is required to view this feature. If you are using an operating system that does not support Flash, we are working to bring you alternative formats. Original Article Long-Term Mortality after Gastric Bypass Surgery Ted D. Adams, Ph.D., M.P.H., Richard E. Gress, M.A., Sherman C. Smith, M.D., R. Chad Halverson, M.D., Steven C.
Simper, M.D., Wayne D. Rosamond, Ph.D., Michael J. LaMonte, Ph.D., M.P.H., Antoinette M. Stroup, Ph.D., and Steven C. N Engl J Med 2007; 357:753-761 DOI: 10.1056/NEJMoa066603.
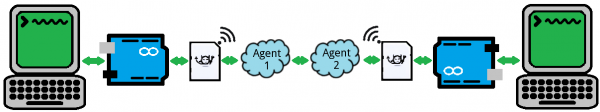
Old Floppy disk Some embroidery machines in commercial use today still use floppy disks and or serial com port connection to upload designs into the embroidery machine memory. However, after some research I managed to find two brands/models that consistently preformed well in customer feedback.
Results During a mean follow-up of 7.1 years, adjusted long-term mortality from any cause in the surgery group decreased by 40%, as compared with that in the control group (37.6 vs. 57.1 deaths per 10,000 person-years, P. Several studies have shown a positive association between obesity and an increased rate of death, with an even greater risk of death among persons with a body-mass index (BMI, the weight in kilograms divided by the square of the height in meters) of 35 or more, as compared with those with a BMI of 30 to 34. However, the evidence is less clear as to whether weight loss reduces mortality. Although substantial and sustained weight loss follows bariatric surgery, limited data are available regarding long-term death rates after such surgery, and available studies have certain methodologic limitations. Elsewhere in this issue of the Journal, the Swedish Obesity Subjects (SOS) study group reports mortality results after surgical intervention for weight loss. However, gastric bypass accounted for only 13% of procedures in the SOS study, whereas 68% of the procedures were vertical banded gastroplasty, which generally results in less weight loss than gastric bypass and is now performed infrequently.
Thus, data on long-term mortality are needed for gastric bypass surgery. In light of the limited long-term data on mortality after bariatric surgery and the recent increase in bariatric surgery in the United States, we undertook a retrospective cohort study to compare long-term (18-year) rates of death from any cause and from specific causes in a large cohort of subjects who had undergone gastric bypass surgery, as compared with a group of severely obese control subjects from the general population in Utah. Study Groups We evaluated subjects for inclusion in two study groups: a consecutive series of 9949 patients who had undergone Roux-en-Y gastric bypass surgery between 1984 and 2002, performed by a single Utah surgical practice of six experienced bariatric surgeons, and 9628 markedly obese adults (with a self-reported BMI of 35 or more) who were randomly selected from among applicants for a driver's license or identification (ID) card. From these groups, we matched 7925 subjects in the surgery group with 7925 subjects in the control group.
This one-to-one matching was based on the following variables: sex, BMI (presurgical measurement in the surgery group and self-reported BMI at the time of the license application, which was corrected for self-reporting bias before matching, as detailed below), and age and year (both at the time of surgery and of license application). Age was matched within 5-year categories, and BMI was matched according to the intervals of 33 to 44, 45 to 54, and 55 or more. Numbers of total and matched subjects for all years are shown in Figure 1 Total Numbers of Subjects and Matched Pairs in the Surgery Group and the Control Group (1984–2002).
The numbers of control subjects are the numbers extracted from either microfilm or electronic records of driver's-license applications in Utah.. Control subjects were identified from records of applications for Utah driver's licenses and state ID cards that were available on microfilm for the years from 1984 to 1994 and in electronic files for the years 1995 to 2002. With the use of microfilm readers, 1,655,094 records were scanned by hand to obtain 16,395 control subjects with a self-reported BMI of 35 or more for the years 1984 to 1994, and 2,610,801 records were searched electronically to obtain 67,062 control subjects for the years 1995 to 2002. Data on height, weight, name, date of birth, sex, application date, and Social Security number were extracted.
There was excellent matching of subjects for the surgery group and the control group with the use of the electronic portion of the driver's license file. However, despite the extraction of 1.6 million microfilm records, the number of identified severely obese control subjects was insufficient to match all subjects in the surgery group for the years 1984 to 1994. To correct for possible error in reporting height and weight on driver's license applications, records of all subjects in the surgery group were compared with the electronic files for their applications for a Utah driver's license. There were 592 matches of subjects in the surgery group (68% of whom were women) whose driver's-license renewal had occurred less than 5 years before their gastric bypass surgery (average, 1.8 years). The BMI of these subjects, calculated in the clinic just before their surgery, was compared with the self-reported BMI on their applications. We then used regression equations of self-reported and measured BMI specific for men and women to correct the self-reported BMI for each driver's license applicant before matching this subject with one in the surgery group (see data in the, which is available with the full text of this article at www.nejm.org).
To minimize the potential for selecting a control subject who had undergone gastric bypass surgery, all driver's-license applicants were screened against the entire surgery group and against a registry of patients who had undergone gastric bypass surgery in Utah hospitals between 1992 and 2002. Potential control subjects matching those in either database of patients who had undergone gastric bypass were eliminated from the follow-up study. To ensure that exclusion of unmatched subjects in the surgery group and the control group did not introduce bias, the rate of death for all subjects was compared with that of the matched subgroup. Control subjects were also rematched to subjects in the surgery group with the use of their self-reported BMI (not their BMI corrected by regression equations) to estimate the magnitude of the effect of the BMI adjustment on mortality. All subjects were linked to the Utah Cancer Registry, part of the National Cancer Institute's Surveillance, Epidemiology, and End Results program, so that additional analyses could be performed excluding prevalent baseline cancer. Because it was unclear how weight loss induced by gastric bypass surgery would improve the short-term risk of death from cancer, additional mortality analysis was performed eliminating all deaths from cancer occurring within the first 5 years after baseline. The percentages of subjects reporting a Social Security number differed between the study groups (86% in the surgery group and 99% in the control group).
To investigate any possible introduction of bias from the use of incomplete matching data for the NDI search, we performed additional analyses that included only subjects with reported Social Security numbers. Finally, analyses were performed comparing mortality within BMI subgroups (. Primary and Secondary Outcomes The primary outcome was death from any cause. Secondary outcomes were death from various specific causes. Causes of death were obtained from the National Death Index (NDI) and categorized with the use of the International Classification of Diseases, Ninth Revision and Tenth Revision (ICD-9 and ICD-10) (Table 1 of the ). The NDI obtains all death-certificate data from all states in the United States.
Data sent to the NDI included name, sex, date of birth, and Social Security number (when available). The most probable matches between subjects in the two study groups and NDI's records were obtained according to the published recommendations from the NDI.
Statistical Analysis We compared the risk of death in the two study groups with the use of Cox proportional-hazards regression analysis. Baseline was defined as the date of gastric bypass surgery or of license application for the control group. Survival time was computed as the difference between the baseline date and the date of death for decedents or January 1, 2003, for survivors. All models included sex, baseline age, year of surgery or license application, and a cubic polynomial of the baseline BMI.
Coefficients for the squares and cubes of age were not significant. Fm 2009 9 3 Keygen Torrent there. Survival curves were produced on the basis of Kaplan–Meier analysis. Differences in mortality among BMI subgroups were tested with the log-rank statistic. Absolute unadjusted death rates are presented as deaths per 10,000 person-years of follow-up. Analyses were completed with the use of SAS software, version 9.1. P values and 95% confidence intervals are two-sided, and a P value of less than 0.05 was considered to indicate statistical significance. Results Table 1 Characteristics of Subjects in the Study Groups (1984–2002).
Shows age, BMI, sex, and death and survival data for all subjects and those in the two matched study groups. There were no significant differences between the study groups in baseline age and average length of follow-up. The mean BMI differed significantly between the matched study groups (45.3 in the surgery group and 46.7 in the control group, P. Discussion In our study, we examined the records of patients who had undergone gastric bypass surgery to determine their long-term risk of death, as compared with that of a population control group in which weight was self-reported. The estimated number of lives saved after a mean follow-up of 7.1 years was 136 per 10,000 gastric bypass surgeries. Despite evidence of an increased risk of death among obese persons, mortality studies of obese subjects who lost weight without surgical intervention have been inconclusive. Bariatric surgery is reported to be the most effective option for weight loss in the severely obese.
Therefore, patients who have undergone bariatric surgery are a promising cohort for exploring the association between the risk of death and weight loss. However, only limited data from studies with varying results are available on long-term mortality after bariatric surgery, and the survival data from the SOS study are only now being reported. In our study, the death rate (2.7%), mean length of follow-up (7.1 years), mean age at entry (39.5 years), and percentage of women (84%) among matched subjects most closely resemble the results reported by Zhang et al. (3.5%, 8.3 years, 38.9 years, and 87%, respectively). Death rates for subjects in control groups that were reported by Flum and Dellinger (16.3%) and Christou et al.
(6.2%) were higher than that in our study (4.1%), a factor that might be related to the use of medical patients as control subjects in the other two studies. However, in this pair of studies, ICD-9 codes indicating morbid obesity were used, but no data were available on BMI, and both studies involved older subjects (47 years, vs.
39 years in our study) and fewer women (64% vs. 84%); in addition, Utah death rates are among the lowest in the United States. Christou et al. Reported that among patients who had undergone gastric bypass surgery, the rate of death from any cause decreased by 89% after a mean follow-up of 2.6 years, as compared with the rate among control subjects. Flum and Dellinger reported a 33% reduction in the rate of death from any cause after gastric bypass surgery, as compared with the rate among control subjects, after a mean follow-up of 4.4 years, which was similar to the adjusted 40% reduction in the rate of death from any cause after 7.1 years in the matched groups in our study. The prospective SOS study showed a reduction in overall mortality in the surgery group, as compared with matched subjects in the control group (adjusted hazard ratio, 0.71; P=0.01). Although only 13% of the subjects in the surgery group of the SOS study underwent gastric bypass surgery, this study showed reduced long-term mortality after surgically induced weight loss.
In our study, during the first year after surgery, 0.53% of subjects in the surgery group died, which was similar to the rate in the control group (0.52%). Despite surgery-specific complications leading to death, the combined risk of death associated with both surgery and obesity did not differ from the rate of death for subjects in the control group. A possible contribution to this low rate of death during the first year is the fact that the center where subjects underwent surgery has performed more than 12,000 gastric bypass operations since 1979. Certain limitations and biases remain in our study. The absence of follow-up medical history prevented us from knowing whether surgical patients entering the medical care system were more aggressively treated for health issues after gastric bypass surgery, perhaps favorably influencing mortality.
However, studies of patients after bariatric surgery have shown a reduction in obesity-related illnesses, suggesting that patients needed less follow-up medical care after surgery. The baseline health status of patients seeking gastric bypass surgery, as compared with that of control subjects, is also unknown. In an ongoing prospective study of complications in 423 subjects who underwent gastric bypass surgery and 321 severely obese control subjects, we have found no significant baseline differences in the smoking history or the presence or absence of hypertension, diabetes, dyslipidemia, or sleep apnea, suggesting that the characteristics of subjects in the two study groups in this mortality study were probably similar at baseline.
Surgeons in this study denied surgery to less than 1% of subjects because of preexisting health conditions, suggesting that a bias with respect to health status was limited to very few patients. It is possible that severely obese persons who did not seek gastric bypass surgery were less likely to make healthy lifestyle choices, resulting in a rate of death higher than that for persons who underwent surgery.
In our study, limiting the comparison of matched subjects in the two study groups to those with available Social Security numbers had little effect on the hazard ratio for death from any cause in the surgery group (0.60 for all matched subjects and 0.63 for all matched subjects with Social Security numbers), suggesting that bias from missing Social Security numbers was minimal. We acknowledge that death certificates are not entirely accurate so that cause-specific hazard ratios may be approximations. However, we assume that errors present on death certificates would be similar in the two groups. Since data on weight at the time of death were not available, we could not analyze the risk of death according to the amount of weight lost.
In addition, only self-reported baseline weight was available for the control group. Studies reporting differences between actual and self-reported height and weight indicate that women are more likely to underreport body weight than are men and that underreporting of weight is greater with increasing BMI. To reduce self-reported BMI bias, we developed sex-specific regression equations for BMI correction. Without BMI correction for the control subjects before matching, the reduction in death from any cause in the surgery group was 46% (Table 4 of the ), as compared with a reduction of 40% with BMI corrected before matching.
The significantly reduced mortality estimates were remarkably robust despite all attempts to investigate and correct for the various weaknesses of the study. The reduction in the risk of death from cancer after a mean follow-up of 7.1 years is surprising. Considerable evidence indicates that an increased risk of cancer is associated with obesity, although the association between a reduced risk of cancer and voluntary weight reduction is less clear. Cancer screening may improve with weight loss, thereby detecting cancers at an earlier stage in the surgery group and improving survival. Analyses of cancer staging in subjects in both study groups are ongoing. However, it is doubtful that possible study biases fully explain the large observed reduction in cancer-related mortality. The reduction in deaths from cancer persisted even after the exclusion of prevalent cancers and deaths from cancer occurring within 5 years after baseline.
Our study suggests that favorable clinical outcomes after gastric bypass surgery translate into significant disease-specific reductions in the risk of death. Despite reductions in disease-related deaths after gastric bypass surgery, the risk of non–disease-related death, such as accidents and suicides, increased by a factor of 1.58, as compared with that in the control group. Reports reveal that a substantial number of severely obese persons have unrecognized presurgical mood disorders or post-traumatic stress disorder or have been victims of childhood sexual abuse. Data on the association between presurgical psychological status and postsurgical outcome are limited. Some centers for bariatric surgery recommend that all patients undergo psychological evaluation and, if necessary, treatment before surgery and psychologically related surveillance postoperatively. Although research has shown an improved quality of life after gastric bypass surgery, certain unrecognized presurgical conditions may reappear after surgery.
The results of our study suggest that further research is warranted to explore the optimal approach to evaluating candidates for surgery, including the possible need for psychological evaluation and psychiatric treatment before surgery, and aggressive follow-up after surgery. Despite certain limitations, our findings indicate that patients who undergo gastric bypass surgery have decreased long-term mortality from any cause and from disease-specific causes but have increased mortality from nondisease causes, as compared with control subjects. Our study provides useful data for patients considering gastric bypass surgery, for medical professionals serving the severely obese population, and for insurance carriers making decisions about whether to cover this procedure. Supported by a grant (DK-55006) from the National Institute of Diabetes and Digestive and Kidney Diseases and a grant (M01-RR00064) from the National Center for Research Resources; by the Utah Cancer Registry, which is funded by a contract (NO1-PC-35141) with the National Cancer Institute; and by the Utah Department of Health and the University of Utah. Smith reports receiving a lecture fee from U.S. No other potential conflict of interest relevant to this article was reported.
We thank bariatric surgeons Dr. Goodman, and the late Dr. Source Information From the Cardiovascular Genetics Division, University of Utah School of Medicine (T.D.A., R.E. Dfi Lanparty Nf4 Sound Driver Windows 7. G., S.C.H.); Intermountain Health and Fitness Institute, LDS Hospital (T.D.A.); Rocky Mountain Associated Physicians (S.C. Smith, R.C.H., S.C. Simper); and Utah Cancer Registry, University of Utah (A.M.S.) — all in Salt Lake City; School of Public Health, University of North Carolina at Chapel Hill, Chapel Hill (W.D.R.); and the Department of Social and Preventive Medicine, University at Buffalo, Buffalo, NY (M.J.L.). Address reprint requests to Dr. Adams at Cardiovascular Genetics, University of Utah School of Medicine, 420 Chipeta Way, Rm.
1160, Salt Lake City, UT 84108,. References • 1 Adams KF, Schatzkin A, Harris TB, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med 2006;355:763-778 • 2 Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA 2005;293:1861-1867 • 3 McTigue K, Larson JC, Valoski A, et al.
Mortality and cardiac and vascular outcomes in extremely obese women. JAMA 2006;296:79-86 • 4 Sorensen TI. Weight loss causes increased mortality: pros. Obes Rev 2003;4:3-7 • 5 Yang D, Fontaine KR, Wang C, Allison DB. Weight loss causes increased mortality: cons. Obes Rev 2003;4:9-16 • 6 National Institutes of Health. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults -- the Evidence Report.
Obes Res 1998;6:Suppl 2:51S-209S[Erratum, Obes Res 1998;6:464.] • 7 MacDonald KG Jr, Long SD, Swanson MS, et al. The gastric bypass operation reduces the progression and mortality of non-insulin-dependent diabetes mellitus. J Gastrointest Surg 1997;1:213-220 • 8 Flum DR, Dellinger EP. Impact of gastric bypass operation on survival: a population-based analysis.
J Am Coll Surg 2004;199:543-551 • 9 Christou NV, Sampalis JS, Liberman M, et al. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients.
Ann Surg 2004;240:416-423 • 10 Zhang W, Mason EE, Renquist KE, Zimmerman MB. Factors influencing survival following surgical treatment of obesity. Obes Surg 2005;15:43-50 • 11 Sjostrom L, Narbro K, Sjostrom CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med 2007;357:741-752 • 12 Sowemimo OA, Yood SM, Courtney J, et al.
Natural history of morbid obesity without surgical intervention. Surg Obes Relat Dis 2007;3:73-77 • 13 Sjostrom L, Larsson B, Backman L, et al. Swedish Obese Subjects (SOS): recruitment for an intervention study and a selected description of the obese state. Int J Obes Relat Metab Disord 1992;16:465-479 • 14 Courcoulas AP, Flum DR. Filling the gaps in bariatric surgical research. JAMA 2005;294:1957-1960[Erratum, JAMA 2005;294:2848.] • 15 Steinbrook R. Surgery for severe obesity.
N Engl J Med 2004;350:1075-1079 • 16 Santry HP, Gillen DL, Lauderdale DS. Trends in bariatric surgical procedures. JAMA 2005;294:1909-1917 • 17 Pope GD, Birkmeyer JD, Finlayson SR. National trends in utilization and in-hospital outcomes of bariatric surgery. J Gastrointest Surg 2002;6:855-860 • 18 Horm J.
Assignment of probabilistic scores to National Death Index record matches. In: Bildgrad R, ed. National Death Index plus: coded causes of death. Hyattsville, MD: Division of Vital Statistics, National Center for Health Statistics, 1996:A5-A12. • 19 Solomon CG, Dluhy RG. Bariatric surgery -- quick fix or long-term solution? N Engl J Med 2004;351:2751-2753 • 20 Wolfe BM, Morton JM.
Weighing in on bariatric surgery: procedure use, readmission rates, and mortality. JAMA 2005;294:1960-1963 • 21 Kushner RF, Noble CA. Long-term outcome of bariatric surgery: an interim analysis. Mayo Clin Proc 2006;81:Suppl 10:S46-S51 • 22 Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA 2004;292:1724-1737[Erratum, JAMA 2005;293:1728.] • 23 Sjostrom L.