Logistic Regression Program Rca
Row and Columns model 2 p rc_spline module to generate restricted cubic splines p rca module to compute various revealed comparative advantage (RCA). To estimate a linear regression model with one interacted high dimensional fixed effect p reglike module to calculate log-likelihood function value from regress p. We would like to show you a description here but the site won’t allow us.
Methods From 1737 patients undergoing PCI between March 2004 and 2005, those with cardiogenic shock, primary PCI, total occlusions, and multivessel or multi-lesion PCI were excluded. Baseline characteristics and in-hospital outcomes were compared in 408 patients with PCI on proximal LAD versus 133 patients with PCI on proximal LCX/RCA (study I) and 244 patients with PCI on non-proximal LAD (study II). From our study populations, 449 patients in study I and 549 patients in study II participated in complete follow-up programs, and long-term PCI outcomes were compared within these groups. The statistical methods included Chi-square or Fisher's exact test, student's t-test, stratification methods, multivariate logistic regression and Cox proportional hazards model. Results In the proximal LAD vs. Proximal LCX/RCA groups, smoking and multivessel disease were less frequent and drug-eluting stents were used more often (p = 0.01, p.
Stenosis of the proximal segment of the left anterior descending coronary artery (LAD) is a special subgroup of coronary artery disease (CAD), given the high-risk profile that these lesions have alone or in the context of multivessel disease [, ]. Patients with proximal LAD occlusion in association with low left ventricular ejection fraction have been reported to have 19-fold higher mortality than the general population [ ]. The data from previous studies suggest that the outcome after revascularization depends on the distribution of prerevascularization coronary artery disease.
In that regard, the severity and location of LAD involvement have been identified as important determinants of outcome in patients with CAD [ ]. This lesion carries a high risk of restenosis after balloon angioplasty with reported patency rate at six month-follow-up of approximately 75% [ ].
However, some studies have shown that stenting may reduce the rate of restenosis in these lesions in comparison with balloon angioplasty [ ]. Specifically, drug-eluting stents have been shown to be related to significantly reduced restenosis rates compared to bare metal stents [, ]. Numerous studies have investigated the outcome of percutaneous coronary intervention (PCI) and bypass surgery in patients with LAD stenosis [,, ]. Generally, the presence of a proximal LAD stenosis has swayed the cardiologists to refer the patients to coronary artery bypass grafting (CABG) presuming these lesions have an overall higher rate of restenosis than proximal left circumflex or right coronary artery [ ].
However, according to the American College of Cardiology/American Heart Association, only type B2/C lesions of the LAD carry a high risk of target vessel revascularization (TVR) and morbidity [ ] and surgery has been proposed as a better option only for such lesions [ ]. Aadhar Card Application Form Free Download Pdf In Tamil. According to the 2003 report from the Iranian Statistical Center, 14100 PCI procedures were performed in 50 hospitals in Iran. Of these, approximately 1700 procedures were carried out in Tehran Heart Center (THC). Because of the clinical significance of the lesions located in proximal LAD, our objective in this study was to evaluate the procedural results, in-hospital and long-term clinical outcomes of PCI on proximal LAD, proximal left circumflex (LCX) or right coronary artery(RCA), and non-proximal LAD.
Study population From a total of 1737 consecutive patients undergoing PCI at THC between March 2004 and March 2005, a patient cohort with PCI for de novo narrowing in the proximal segments of coronary arteries or non-proximal LAD were included in the study. Patients with cardiogenic shock, primary PCI, total occlusions, and multivessel or multi-lesion PCI were excluded. Among the 785 remaining patients: 408 had PCI on proximal LAD, 133 underwent PCI on proximal LCX or RCA, and 244 patients were treated with PCI on non-proximal LAD. In study I (n = 541), we compared the outcomes of PCI on proximal LAD versus proximal LCX/RCA. In study II (n = 652), the outcome of PCI on proximal LAD versus non-proximal LAD were compared. Baseline, clinical, angiographic, and procedural characteristics plus in-hospital outcomes were obtained by research physicians and entered into a computerized database by computer operators. Finally, 449 patients in study I and 549 patients in study II agreed to participate in follow-up programs.
They were monitored by cardiologists 1, 5, and 9 months post angioplasty and once a year thereafter. Patient follow up was done in the clinic or by formal telephone interviews. Clinical data obtained were: major adverse cardiac events (MACE), including cardiac death, non-fatal myocardial infarction (MI), and TVR (CABG or repeated PCI). The data were recorded in data sheets and later transferred into a computerized database.
This study was approved by the THC Ethics Committee. Informed consent was obtained from patients before enrolment into this study. Definitions Patients already taking hypertensive medication or those whose average of two blood pressure readings at least five minutes apart in the sitting posture was ≥ 140/90 mmHg were labeled as hypertensive [ ]. Patients with a history of taking antihyperlipidemic drugs, total cholesterol ≥ 200 mg/dl or low density lipoprotein ≥ 130 mg/dl were defined as hypercholestrolemic [ ]. Diabetes mellitus was diagnosed to be present if a patient had a definite history of treated diabetes, fasting plasma glucose ≥ 126 mg/dl or two-hour post-load glucose ≥ 200 mg/dl, based on the guidelines of the American Diabetes Association [ ]. Angina symptoms were defined according to the classification of the Canadian Cardiovascular Society [ ]. Lesion types were noted according to the American College of Cardiology/American Heart Association (ACC/AHA) lesion characteristics classification [ ].
Left ventricular ejection fraction was obtained from cardiac catheterization ventriculograms. Q wave MI was defined as the presence of new Q waves in post-procedure electrocardiograms with a 3-fold increase in MB fraction of creatinine kinase. Non-Q wave MI was defined as a 3-fold increase in MB fraction of creatinine kinase without the development of new Q waves [ ].
Angiographic success was defined as residual stenosis. Statistical testing was performed by chi-square test or Fisher's exact test (2-tailed) for categorical variables. Student's t-test was used for comparison of continuous variables. Because of the imbalances in some baseline characteristics, the main study results were confirmed by means of stratified analyses and multivariate logistic regression models. Stratification was performed for variables that either had significant imbalance between the groups (p. Proximal LAD n = 408 Proximal LCX/RCA n = 133 P value (study I) * Non-proximal LAD n = 244 P value (study II) ** Age(yrs) (mean ± SD) 55.36 ± 10.87 56.94 ± 9.7 0.14 55.6 ± 10.88 0.78 Male 285(69.9%) 104(78.2%) 0.06 163(66.8%) 0.41 Diabetes Mellitus 76(19.1%) 33(25.4%) 0. 12 58 (24%) 0.14 Family history of CAD 89(21.8%) 21(15.8%) 0.13 54(22.1%) 0.91 hypercholesterolemia 171(43%) 59(45.4%) 0.63 107(44.2%) 0.76 Current smoker 157(38.5%) 68(51.1%) 0.01 86(35.2%) 0.41 hypertension 132(33.2%) 38(29.2%) 0.4 92(38%) 0.21 Myocardial infarction 138 (33.8%) 38 (28.6%) 0.26 72 (29.5%) 0.25 Prior PCI (Non-target vessel) 15(3.7%) 12(9%) 0.01 7(2.9%) 0.58 Prior CABG 2(0.5%) 2(1.5%) 0.24 1(0.4%) >0.999.
Proximal LAD n = 408 Proximal LCX/RCA n = 133 P value (study I) * Non-proximal LAD n = 244 P value (study II) ** Angiographic characteristics Multivessel disease 110 (33.1%) 64 (61.5%) 45°) 9 (2.2%) 18 (13.5%). Baseline characteristics Table represents selected baseline characteristics of patients treated for proximal stenoses of major epicardial arteries and non-proximal LAD. Current smoking and prior non-target vessel PCI had a lower frequency in patients with PCI on proximal LAD versus LCX or RCA. However, in patients with PCI on proximal versus non-proximal LAD, the baseline demographic characteristics did not differ. Mean Ejection Fraction was 53.54 ± 9.45% in the proximal LAD versus 53.12 ± 10.24% and 54.35 ± 9.22% in the proximal LCX/RCA and non-proximal LAD groups (p = NS), respectively. In the proximal LAD versus proximal LCX/RCA and non-proximal LAD, the frequency of unstable angina (33.7% vs.
34.8% and 33.7%) and prior MI (33.8% vs. 28.6% and 29.5%) had no statistically significant difference (P = NS). Angiographic and procedural characteristics (Table ) Frequency of type B2/C lesions was similar in the proximal LAD vs. Proximal LCX/RCA and non-proximal LAD groups: (42.8% vs.43.8% and 47.8, p = NS). Multivessel disease and angulated segments were less frequent in the proximal LAD group. In the proximal LAD versus proximal LCX/RCA group, lesions were longer (16.89 ± 8.1 mm versus 14.68 ± 7.38 mm, p = 0.007) and had lower frequency of proximal segment tortuosity (p = 0.03). However, percentage of lesions smaller than 3 mm in diameter did not differ.
On the other hand, in the proximal versus non-proximal LAD group, expectedly, lesions had larger reference vessel diameters. Stents were used in 99.8% of patients in the proximal LAD versus 98.5% in the proximal LCX/RCA (p = NS) and 96.7% in the non-proximal LAD groups (p = 0.002). Pre- and post-procedural stenosis percentages did not differ significantly in the proximal LAD versus proximal LCX/RCA and non-proximal LAD groups (89.44 ± 8.65% versus 89.15 ± 9.37% and 89.96 ± 8.28%; 0.65 ± 3.24% versus 2.75 ± 13.69% and 1.11 ± 4.51%, p = NS).
Patients with PCI on proximal LAD versus proximal LCX/RCA were more commonly treated with drug-eluting stents and had longer stents with smaller diameters. Patients with proximal versus non-proximal LAD stenosis were more often treated with stents, especially the direct stenting technique. In-hospital and late clinical outcomes. In the proximal LAD group, procedures were angiographically successful in 100% of cases, which was significantly greater than the other two groups. In-hospital events, which occurred only as non-Q wave MI in our cohort, were observed in 8 (2%) in the proximal LAD group, while only 1 patient in the proximal LCX/RCA and non-proximal LAD group (0.8% and 0.4% respectively) displayed such symptoms(P = NS). Procedural success rates were similar in both comparisons (table ). Mean follow-up duration was 10.81 ± 3.69 months in total population.
Major adverse cardiac events at 9-month follow-up, including cardiac death, MI, and TVR (CABG or repeated PCI) were not significantly different in the proximal LAD versus the other two groups (table ). After stratification for factors that either had significant imbalance between the groups or were clinically important, the MACE rates in the proximal LAD versus proximal LCX/RCA and non-proximal LAD groups were still comparable (table ). Similarly, in multivariate logistic regression models, there was no difference in MACE rates in the proximal LAD versus proximal LCX/RCA (p = 0.85, 95% CI = 0.19–3.89, OR = 0.87) and proximal versus non-proximal LAD groups (p = 0.66, 95% CI = 0.29–2.1, OR = 0.8). Cox proportional hazards model also did not show any difference in MACE-free survival rates at long-term follow-up (figure ). The main finding that emerges from this study is that long-term outcomes of PCI including MACE in patients with proximal LAD stenosis are similar to patients with proximal LCX or RCA and non-proximal LAD stenosis. Also worth noting from our findings was that angiographic success was higher in patients with proximal LAD stenosis.
Management of proximal coronary artery disease is important due to the large areas of myocardium that lie downstream of the stenoses. The proximal LAD artery stenosis represents the most important proximal site for obstructive coronary artery after left main stem lesion disease, as it supplies 40%–50% of the total left ventricular myocardium and could result in ischemia to a large area of myocardium [, ].
Moreover, Patients with a critical stenosis of the proximal LAD segment are particularly prone to adverse effects of MI and, therefore, require a safe and long-term effective method of treatment [ ]. Previous studies have demonstrated that interventional treatment produces are more beneficial than pharmacological treatment in severe proximal LAD artery disease [ ]. However, The results of nonstenting PCI to proximal LAD stenoses has been less satisfactory than procedures in the proximal right/circumflex coronary arteries due to higher rates of restenosis in this area [,, ]. Stenting leads to better clinical outcomes than percutaneous transluminal coronary angioplasty in the treatment of isolated lesions of proximal LAD by reducing the risk of restenosis by about 50% [ ]. In fact, stenting of lesions in the proximal LAD is as effective and safe as treatment of lesions located in distal LAD. Therefore, in the current stenting era, location of the lesion in the LAD is not predictive of worse outcome. Furthermore, when stenting is feasible, it may not be taken into account in the choice of revascularization strategy [ ].
However, the re-intervention rates have been higher after bare-metal stenting than bypass surgery of the proximal LAD [ ]. With the advent of drug-eluting stents, a reduction has been achieved in restenosis rates after stenting in proximal LAD. This in turn has narrowed the 'reintervention gap' between drug-eluting stents enough to eliminate the major advantage of bypass surgery for the treatment of LAD disease [ ]. In our study, no significant difference was observed in rates of major adverse cardiac events during long-term follow-up in the proximal LAD versus the other two groups. Even after adjusting for factors such as stents, particularly drug-eluting stents, which were used most frequently in the proximal LAD group, no statistical difference was detectible. MACE-free survival rates were also similar between the groups (figure ). Before our study, Ashby et al had studied the outcomes of stenting in proximal LAD versus proximal LCX/RCA [ ].
In their study, multivariate analysis was conducted to adjust these groups for some baseline differences. However, the main endpoint of this study i.e. Rate of TLR, was still similar in both groups in patients treated with stents.
Before that, The Stent Restenosis (STRESS) study had shown that irrespective of the procedure used (balloon angioplasty or stenting), the most important predictors of the larger luminal diameter at follow-up were the size of the luminal diameter after the procedure, the initial reference vessel diameter, and the location of a lesion in a vessel other than LAD [ ]. As a secondary aim, we found that angiographic success rate was higher in patients with proximal LAD stenoses. This may be attributed to better accessibility of lesions and higher frequency of stent use in the proximal LAD group. However, because of the paucity of procedural failure rates, this effect could not be proven by means of statistical analyses. One of the limitations of this study was the relatively small sample size of patients who had developed complications, which made it difficult to determine the predictors of MACE from the multivariate analysis. On the other hand, we had to exclude patients with multi-lesion or multivessel percutaneous coronary intervention, because otherwise we would not have been able to attribute MACE to a particular lesion site.
Acknowledgements We are grateful to Mahmood Sheikh Fathollahi for assisting us in statistical analyses. This study was funded by Tehran Heart Center, which had role in data collections and preparation of datasets for patients. The authors were funded by the research department of Tehran Heart Center, Medical Sciences/University of Tehran. Competing interests The author(s) declare that they have no competing interests. Authors' contributions MA designed the study, contributed substantially to the interpretation of data and progression of work, and gave the final approval for publication.
MRD conducted the data collection and statistical analyses, and participated in writing of the paper. MA, SEK, AHZ, and MS equally performed the angioplasty procedures and contributed to the interpretation of results. All authors read and approved the final manuscript. Supplementary material. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT, Roccella EJ, Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee: Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. 2003, 42: 1206-52.
Adobe Flash Player is required to view this feature. If you are using an operating system that does not support Flash, we are working to bring you alternative formats. Original Article Delayed Time to Defibrillation after In-Hospital Cardiac Arrest Paul S. Chan, M.D., Harlan M.
Krumholz, M.D., Graham Nichol, M.D., M.P.H., Brahmajee K. Nallamothu, M.D., M.P.H., and the American Heart Association National Registry of Cardiopulmonary Resuscitation Investigators N Engl J Med 2008; 358:9-17 DOI: 10.1056/NEJMoa0706467.
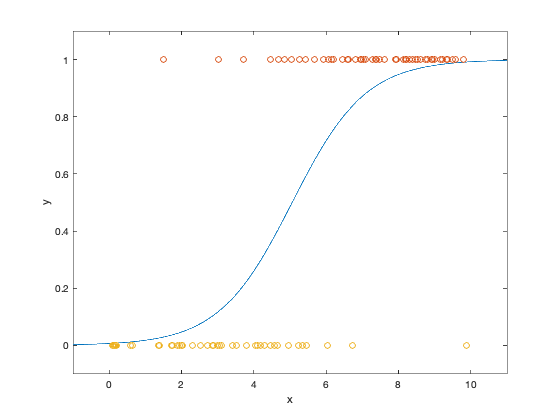
Methods We identified 6789 patients who had cardiac arrest due to ventricular fibrillation or pulseless ventricular tachycardia at 369 hospitals participating in the National Registry of Cardiopulmonary Resuscitation. Using multivariable logistic regression, we identified characteristics associated with delayed defibrillation. We then examined the association between delayed defibrillation (more than 2 minutes) and survival to discharge after adjusting for differences in patient and hospital characteristics.
Results The overall median time to defibrillation was 1 minute (interquartile range. Between 370,000 and 750,000 hospitalized patients have a cardiac arrest and undergo cardiopulmonary resuscitation each year in the United States, with less than 30% expected to survive to discharge. Among the leading causes of cardiac arrest among adults during a hospitalization are ventricular fibrillation and pulseless ventricular tachycardia from primary electrical disturbances or cardiac ischemia. In contrast to cardiac arrests due to asystole or pulseless mechanical activity, survival from cardiac arrests due to ventricular fibrillation or pulseless ventricular tachycardia is improved if defibrillation therapy is administered rapidly. Current recommendations are that hospitalized patients with ventricular fibrillation or pulseless ventricular tachycardia should receive defibrillation therapy within 2 minutes after recognition of cardiac arrest.
Previous studies have suggested an association between time to defibrillation and survival, but the inclusion of cardiac arrests not amenable to defibrillation in most studies remains a potential confounder of this association. Moreover, the extent to which delayed defibrillation occurs in U.S. Hospitals and its potential effect on survival are unclear. Accordingly, we examined how often delayed defibrillation occurred during in-hospital cardiac arrests caused by ventricular arrhythmias and investigated the relationship between delayed defibrillation and survival, using data from the National Registry of Cardiopulmonary Resuscitation (NRCPR). The NRCPR is a large registry of U.S.
Hospitals that uses standardized Utstein definitions (a template of uniform reporting guidelines developed by international experts) to assess both processes of care and outcomes during in-hospital cardiac arrests. It provides a unique resource for exploring these questions as well as identifying key patient and hospital characteristics associated with delayed defibrillation. Study Design The study design of the NRCPR has been described in detail.
Briefly, the NRCPR is a prospective, multicenter registry of in-hospital cardiac arrests that collects data according to standardized Utstein definitions. Cardiac arrest is defined as cessation of cardiac mechanical activity as determined by the absence of a palpable central pulse, apnea, and unresponsiveness. The NRCPR protocol specifies that all consecutive patients with cardiac arrests and without do-not-resuscitate orders be screened by dedicated staff at participating hospitals. Cases are identified by centralized collection of cardiac-arrest flow sheets, reviews of hospital paging-system logs, routine checks for use of code carts (carts stocked with emergency equipment), and screening for code-cart charges from hospital billing offices.
Accuracy of data in the NRCPR is ensured by certification of research staff, use of case-study methods for newly enrolled hospitals before submission of data, and a periodic reabstraction process, which has been demonstrated to have a mean error rate of 2.4% for all data. All patients are assigned a unique code during a single hospitalization, and data are transmitted to a central repository (Digital Innovation) without identification of the patient. Oversight of data collection and analysis, integrity of the data, and research is provided by the American Heart Association.
The institutional review board of the University of Michigan Medical School approved this study and waived the requirement for written informed consent. Patient Population Our analysis included 369 acute care hospitals that provided data for at least 6 months between January 1, 2000, and July 31, 2005.
In patients 18 years of age or older, we identified 14,190 cases of in-hospital cardiac arrest in which the first identifiable rhythm was ventricular fibrillation or pulseless ventricular tachycardia ( Figure 1 Study Cohort. Of the initial 14,190 cases of in-hospital cardiac arrest due to pulseless ventricular tachycardia or ventricular fibrillation listed in the National Registry of Cardiopulmonary Resuscitation, 6789 eligible patients were included in the final study population. If a patient had multiple cardiac arrests during the same hospitalization, we excluded data from subsequent episodes (involving 1587 recurrent arrests) to focus on the index event. We also limited our study population to patients whose cardiac arrests occurred while they were in intensive care units (ICUs) or inpatient beds. Because of the distinctive clinical circumstances associated with other hospital environments, we excluded a total of 3291 patients who were in emergency departments, operating rooms, procedure areas (cardiac catheterization, electrophysiology, and angiography suites), and postprocedural areas at the time of their cardiac arrest.
Finally, we excluded patients with implantable cardioverter–defibrillators (170 patients), those who were receiving intravenous infusions of acute cardiac life support protocol medications for pulseless ventricular tachycardia or ventricular fibrillation (epinephrine, amiodarone, lidocaine, or procainamide) at the time of cardiac arrest (1565 patients), and patients for whom data on the time of the cardiac arrest or defibrillation were missing (766 patients) or inconsistent (22 patients). The patients who were excluded because of missing or inconsistent time data had baseline characteristics that were similar to those of patients in the final study cohort, except that the excluded patients had lower rates of previous myocardial infarction (21.2% vs. Time to Defibrillation The time to defibrillation was calculated as the interval from the reported time of initial recognition of the cardiac arrest to the reported time of the first attempted defibrillation.
Both reported times were determined from cardiac-arrest documentation in the patient's medical records and recorded in minutes. In our primary analysis, we used these data to determine the proportion of study subjects with delayed defibrillation, which was defined as a time to defibrillation greater than 2 minutes. In addition, we classified the study subjects according to whether their defibrillation time was 1 minute or less, 2 minutes, 3 minutes, 4 minutes, 5 minutes, 6 minutes, or more than 6 minutes. End Points The primary outcome for our analysis was survival to hospital discharge. We also evaluated three secondary outcomes: return of spontaneous circulation for at least 20 minutes after onset of the cardiac arrest, survival at 24 hours after the cardiac arrest, and neurologic and functional status at discharge. Neurologic and functional status were assessed among survivors to discharge according to previously developed performance categories. For both neurologic and functional status, outcomes were categorized as no major disability, moderate disability, severe disability, or coma or vegetative state; data on these outcomes were available for 84% of survivors to hospital discharge.
Patients whose data were missing did not differ significantly from those without missing data with regard to likelihood of delayed defibrillation (19.5% vs. 19.1%, P=0.85). Statistical Analysis Unadjusted analyses evaluated baseline differences between patients with and without delayed defibrillation using Student's t-test for continuous variables and the chi-square test for categorical variables. Multivariable logistic-regression models were used to examine the relationship between individual baseline characteristics and delayed defibrillation. Multivariable models were then created to investigate the relationship between delayed defibrillation and outcomes.
All models included age, sex, race (white, black, Hispanic, Asian or Pacific Islander, or Native American), and time to defibrillation (delayed or not delayed) as covariates. Additional candidate variables were selected from the following list after they had been determined to have a significant univariate association (P. Results We identified 6789 patients from 369 hospitals who had in-hospital cardiac arrests due to ventricular fibrillation (69.7%) or pulseless ventricular tachycardia (30.3%). Overall, the median time to defibrillation was 1 minute (interquartile range. Discussion We found that 30.1% of patients with cardiac arrests due to ventricular arrhythmia underwent defibrillation more than 2 minutes after initial recognition of their cardiac arrest, a delay that exceeds guidelines-based recommendations. Sketchup 8 Vray Download Full.
Patients with delayed defibrillation were significantly less likely to survive to hospital discharge. Among survivors, patients with delayed defibrillation were less likely to have no major disabilities in neurologic or functional status. These findings support the conclusion that rapid defibrillation is associated with sizable survival gains in these high-risk patients.
Furthermore, we found a graded association between poorer survival and longer times to defibrillation, even for times beyond 2 minutes. These observations reinforce the rationale for efforts to shorten the time to defibrillation as much as possible to maximize the effectiveness of resuscitation of patients with ventricular fibrillation or pulseless ventricular tachycardia. Our work confirms and extends the findings of other investigations that have shown a relationship between defibrillation time and survival. Although earlier studies linked delayed defibrillation to poorer survival in hospitalized patients, most of these reports included heterogeneous study populations (i.e., both patients with “shockable” and those with “unshockable” rhythms, such as asystole, at the time of cardiac arrest). Moreover, these studies were generally small and involved a limited number of hospitals.
In contrast, our analysis focused only on patients with cardiac arrest due to ventricular fibrillation or pulseless ventricular tachycardia and excluded other potentially inappropriate patients, such as those receiving concomitant treatment with intravenous antiarrhythmic or vasoactive infusions or those with preexisting implantable cardioverter–defibrillators. The large size of the NRCPR and its use of standardized definitions were instrumental in this regard. Several factors related to the hospital setting were associated with delayed defibrillation, including the occurrence of a cardiac arrest after hours or in an unmonitored inpatient bed. These findings imply that response times may be related, in part, to the emergent availability of trained medical personnel, access to defibrillation equipment, and delays in recognition of a ventricular arrhythmia. In addition to hospital-related factors, certain patient characteristics were found to be associated with a greater likelihood of delayed defibrillation. The relationship between a cardiac admitting diagnosis and shorter time to defibrillation is probably due to earlier recognition of the ventricular arrhythmia. However, the association of black race with delayed defibrillation is not intuitively obvious and raises potential issues of disparities in care.
Further studies are warranted to determine whether such variations are due to geographic differences in access to hospitals with more resources (such as more monitored beds) or whether they reflect actual differences in practice patterns according to race. Our study should be interpreted in the context of the following limitations. First, although data available in the NRCPR allowed us to adjust for key variables that have been linked to survival after cardiac arrest, our study used an observational design, and there are variables that we did not or could not capture (for example, a physician's a priori assessment of the likelihood of survival or good neurologic outcome in an arrest).
These additional factors may influence time to defibrillation, leading to residual confounding. Second, data on time to defibrillation relied on reported times of cardiac arrest and defibrillation from hospital records. The use of multiple clocks and the lack of synchronization between the timing of cardiac monitors and defibrillators within a hospital may lead to variability and discrepancies in calculating time to defibrillation. This variability in measurement would be expected to bias our findings toward the null hypothesis, suggesting that we may be underestimating the association between delayed defibrillation and survival.
In addition, because time to defibrillation was recorded in minutes, our analysis primarily explored its association with survival at the skewed upper end of this variable's distribution. The effect of time to defibrillation within short intervals of less than a minute could not be assessed. Third, the results related to neurologic and functional status should be interpreted with caution, since these data were missing for 16% of patients surviving to hospital discharge. Finally, although hospitals in the NRCPR represent nearly 15% of the large hospitals (>250 beds) in the United States, their participation is voluntary. Performance characteristics, quality of care, and survival outcomes may be different in nonparticipating hospitals. In conclusion, we found that delays in the time to defibrillation are common in hospitalized patients with cardiac arrest due to a ventricular arrhythmia, and we identified several patient- and hospital-related factors associated with delayed time to defibrillation. In our analysis, such delays were associated with substantially worse clinical outcomes, with each additional minute of delay resulting in worse survival.
Supported in part by a Cardiovascular Multidisciplinary Research training grant from the National Institutes of Health (NIH) and the Ruth L. Kirchstein Service Award (to Dr. Chan) and by a Clinical Research Scholar Program grant from the NIH (K12 RR017607-01, to Dr.
Nichol reports receiving consulting fees from InnerCool, Paracor Medical, and Northfield Laboratories; receiving travel compensation from Radiant Medical; receiving research grant funding from Medtronic; and having served on advisory boards to the American Heart Association, the National Registry of Cardiopulmonary Resuscitation, and the Medic One Foundation. No other potential conflict of interest relevant to this article was reported. Timothy Hofer for his insightful comments and suggestions on the manuscript. References • 1 Eisenberg MS, Mengert TJ.
Cardiac resuscitation. N Engl J Med 2001;344:1304-1313 • 2 Ballew KA, Philbrick JT. Causes of variation in reported in-hospital CPR survival: a critical review. Resuscitation 1995;30:203-215 • 3 Nadkarni VM, Larkin GL, Peberdy MA, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults.
JAMA 2006;295:50-57 • 4 Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation 2003;58:297-308 • 5 Ewy GA, Ornato JP. 31st Bethesda Conference: emergency cardiac care -- task force 1: cardiac arrest. J Am Coll Cardiol 2000;35:832-846 • 6 Cummins RO, Ornato JP, Thies WH, Pepe PE. Improving survival from sudden cardiac arrest: the “chain of survival” concept: a statement for health professionals from the Advanced Cardiac Life Support Subcommittee and the Emergency Cardiac Care Committee, American Heart Association.
Circulation 19-1847 • 7 Fredriksson M, Aune S, Thoren AB, Herlitz J. In-hospital cardiac arrest -- an Utstein style report of seven years experience from the Sahlgrenska University Hospital. Resuscitation 2006;68:351-358 • 8 Herlitz J, Aune S, Bang A, et al.
Very high survival among patients defibrillated at an early stage after in-hospital ventricular fibrillation on wards with and without monitoring facilities. Resuscitation 2005;66:159-166 • 9 Hajbaghery MA, Mousavi G, Akbari H.
Factors influencing survival after in-hospital cardiopulmonary resuscitation. Resuscitation 2005;66:317-321 • 10 Skrifvars MB, Rosenberg PH, Finne P, et al. Evaluation of the in-hospital Utstein template in cardiopulmonary resuscitation in secondary hospitals. Resuscitation 2003;56:275-282 • 11 Cummins RO, Chamberlain D, Hazinski MF, et al. Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: the in-hospital `Utstein style.'
Circulation 19-2239 • 12 Cummins RO, Sanders A, Mancini E, Hazinski MF. In-hospital resuscitation: executive summary.
Ann Emerg Med 1997;29:647-649 • 13 Jacobs I, Nadkarni V, Bahr J, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa).
Circulation 2004;110:3385-3397 • 14 Zaritsky A, Nadkarni V, Hazinski MF, et al. Recommended guidelines for uniform reporting of pediatric advanced life support: the pediatric Utstein style: a statement for healthcare professionals from a task force of the American Academy of Pediatrics, the American Heart Association, and the European Resuscitation Council. Circulation 19-2020 • 15 Zaritsky A, Nadkarni V, Hazinski MF, et al. Recommended guidelines for uniform reporting of pediatric advanced life support: the pediatric Utstein style: a statement for healthcare professionals from a task force of the American Academy of Pediatrics, the American Heart Association, and the European Resuscitation Council. Resuscitation 1995;30:95-115 • 16 Jennett B, Bond M.
Assessment of outcome after severe brain damage. Lancet 1975;1:480-484 • 17 Castren M, Kurola J, Nurmi J, Martikainen M, Vuori A, Silfvast T. Time matters; what is the time in your defibrillator?
An observational study in 30 emergency medical service systems. Resuscitation 2005;64:293-295 • 18 Kaye W, Mancini ME, Truitt TL.
When minutes count -- the fallacy of accurate time documentation during in-hospital resuscitation. Resuscitation 2005;65:285-290 . Citing Articles • 1 Lauren E Thompson, Paul S Chan, Fengming Tang, Brahmajee K Nallamothu, Saket Girotra, Sarah M Perman, Somnath Bose, Stacie L Daugherty, Steven M Bradley.. (2018) Long-Term Survival Trends of Medicare Patients After In-Hospital Cardiac Arrest: Insights from Get With The Guidelines-Resuscitation ®. Resuscitation 123, 58-64. Emergency Drugs and Equipment. Sedation, 442-455.
• 3 Robert J. Myerburg, Jeffrey J. Sudden Cardiac Death in Adults.
Cardiac Electrophysiology: From Cell to Bedside, 937-948. (2018) Management of cardiac arrest following cardiac surgery. BJA Education 18:1, 16-22. • 5 Anant Mandawat, Aditya Mandawat, Gregory Curfman, L. Kristin Newby..
(2017) A “Shocking” New Code Status. American Heart Journal. • 6 Chih-Hung Wang, Chien-Hua Huang, Wei-Tien Chang, Min-Shan Tsai, Ping-Hsun Yu, Yen-Wen Wu, Wen-Jone Chen..
(2017) Outcomes of adults with in-hospital cardiac arrest after implementation of the 2010 resuscitation guidelines. International Journal of Cardiology 249, 214-219.
• 7 Jonathan Brand, Andrew McDonald, Joel Dunning..